A routine blood test shows elevated WBC—what now? That number on your report can feel alarming, especially if it’s flagged as high. Elevated WBC ICD-10 codes help doctors document and communicate this finding accurately, but the real story lies in what the elevation means for your health.
Many people first learn about high white blood cells (leukocytes) during a complete blood count (CBC) ordered for fatigue, fever, or a general check-up. In most cases, it’s a normal response—your body fighting something off. But sometimes, it signals something more serious that needs attention.
At Prime Hospital Panipat, our hematology and general medicine teams frequently explain these results to worried patients. The good news? Most elevations are temporary and treatable once the cause is found. Let’s walk through everything you need to know about elevated WBC ICD-10 codes, what causes high counts, how it feels, how doctors investigate, and what treatment looks like—step by step, in clear terms.
Elevated WBC ICD-10: The Main Code and What It Really Means
The primary ICD-10 code for elevated WBC (white blood cell count) in 2026 is D72.829 — Elevated white blood cell count, unspecified. This billable code falls under Chapter 3 of ICD-10-CM: Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism.
Doctors use D72.829 when lab results show a high WBC count, but the exact type or cause isn’t specified yet. It’s also listed as leukocytosis, unspecified in many coding resources.
Why “unspecified”? Because leukocytosis simply means more white blood cells than normal—typically above 11,000 cells per microliter (μL) in adults. The normal range is roughly 4,000–11,000/μL, but it varies by age, lab, and individual factors. Newborns can have much higher counts without concern.
Subcategories under D72.82 provide more detail when known:
- D72.820 — Lymphocytosis (symptomatic) — High lymphocytes.
- D72.821 — Monocytosis (symptomatic) — High monocytes.
- D72.822 — Plasmacytosis — Elevated plasma cells.
- D72.823 — Leukemoid reaction — Extreme reactive elevation mimicking leukemia.
- D72.824 — Basophilia — High basophils.
- D72.825 — Bandemia — High band neutrophils.
- D72.828 — Other elevated white blood cell count.
- D72.829 — Unspecified (the catch-all when details are pending).
These codes help with accurate billing, tracking, and research. They exclude eosinophilia (D72.1) and leukemia (C91–C95), which have their own specific codes.
Coding matters because it ensures proper reimbursement, supports medical records, and guides follow-up care. If a specific cause (like infection or leukemia) is confirmed, the primary code shifts to that condition, with D72.829 as secondary.
What Exactly Is Leukocytosis? Defining Elevated WBC
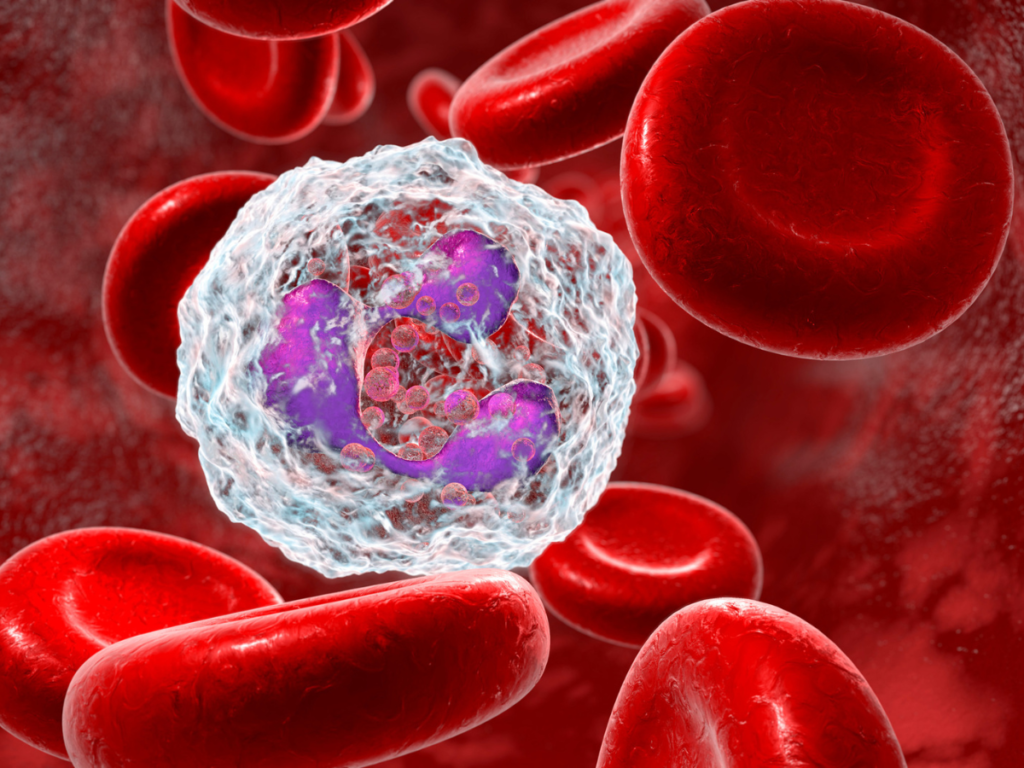
Leukocytosis is the medical term for a high white blood cell count. White blood cells are your immune system’s frontline fighters—they detect and destroy bacteria, viruses, fungi, parasites, and abnormal cells.
There are five main types:
- Neutrophils (50–70% of WBCs) — Fight bacteria and fungi.
- Lymphocytes (20–40%) — Handle viruses and produce antibodies.
- Monocytes (2–8%) — Clean up debris and fight chronic infections.
- Eosinophils (1–4%) — Target parasites and allergies.
- Basophils (<1%) — Involved in allergic reactions.
An elevation can involve one type (e.g., neutrophilia) or all. Hyperleukocytosis (over 100,000/μL) is rare and serious, often linked to leukemia and risking blood thickening (leukostasis).
In adults, counts above 11,000/μL trigger concern; in children, thresholds are higher. Pregnancy and newborns naturally have elevated counts.
Common Causes of Elevated WBC: From Everyday to Serious
The vast majority of elevated WBC cases are reactive—your body responding to a trigger.
Infectious Causes (Most Common) Bacterial infections (pneumonia, urinary tract infections, abscesses) cause neutrophilia. Viral infections (like flu or COVID) raise lymphocytes. Fungal or parasitic infections boost eosinophils or monocytes.
Inflammatory and Autoimmune Conditions Rheumatoid arthritis, lupus, inflammatory bowel disease, vasculitis, and other chronic inflammations drive persistent elevations.
Stress and Physiological Responses Physical/emotional stress, intense exercise, surgery, trauma, burns, seizures, or even labor can spike counts temporarily (often neutrophilia).
Medications and Treatments Corticosteroids (prednisone), lithium, epinephrine, colony-stimulating factors, and certain asthma drugs raise WBCs.
Smoking and Lifestyle Factors Chronic smoking causes mild persistent leukocytosis.
Pregnancy Counts naturally rise (up to 15,000/μL or more) due to physiological stress.
Malignancies Leukemia (acute or chronic), lymphoma, and other cancers (especially metastatic) cause dangerous elevations, often with abnormal cells on smear.
Other Rare Causes Splenectomy (spleen removal), asplenia, allergic reactions, tissue damage, or hereditary conditions.
Reactive leukocytosis usually resolves when the trigger is addressed; malignant causes do not.
Symptoms: What Does Elevated WBC Feel Like?
Leukocytosis itself rarely causes symptoms—the elevation is a lab finding. Symptoms come from the underlying cause.
Common associated signs:
- Fever, chills, night sweats (infection or malignancy).
- Fatigue, weakness, or feeling unwell.
- Frequent infections or slow healing.
- Unexplained weight loss, loss of appetite.
- Easy bruising/bleeding (if platelets affected).
- Bone pain, swollen lymph nodes (serious cases).
- Shortness of breath, headache, vision changes (in hyperleukocytosis).
Mild elevations may cause no symptoms at all—discovered incidentally.
Diagnosis: How Doctors Investigate Elevated WBC
Diagnosis starts with history, physical exam, and lab review.
Step 1: Complete Blood Count (CBC) with Differential Measures total WBC and percentages of each type. Flags abnormalities.
Step 2: Repeat Testing Confirms elevation (transient spikes are common).
Step 3: Blood Smear (Peripheral Smear) Examines cell shapes—blasts suggest leukemia; toxic changes suggest infection.
Additional Tests
- Inflammatory markers (CRP, ESR).
- Cultures (blood, urine, throat) for infection.
- Imaging (chest X-ray, CT) for hidden sources.
- Bone marrow biopsy (if malignancy suspected).
- Flow cytometry or genetic tests (for leukemia/lymphoma).
Doctors rule out reactive causes first before suspecting serious disease.
Treatment: Addressing the Root Cause
There’s no direct “treatment” for elevated WBC—focus is on the underlying condition.
For Infections Antibiotics (bacterial), antivirals, antifungals, or supportive care.
For Inflammation/Autoimmune Anti-inflammatory drugs, steroids, immunosuppressants.
For Medications Adjust or stop the offending drug.
For Stress/Physiological Often resolves spontaneously.
For Malignancy Chemotherapy, targeted therapy, radiation, stem cell transplant—depending on type.
Supportive Care Hydration, rest, pain relief. In severe hyperleukocytosis, leukapheresis (removing WBCs) may be needed.
Most reactive cases resolve in days to weeks with proper care.
When to Seek Help: Red Flags for Elevated WBC
Contact a doctor promptly if:
- Persistent fever >100.4°F.
- Unexplained weight loss or night sweats.
- Severe fatigue or weakness.
- Easy bruising/bleeding.
- Swollen lymph nodes.
- Shortness of breath or confusion.
Routine CBCs catch many cases early—don’t ignore abnormal results.
Conclusion: Elevated WBC ICD-10 Is a Signal, Not a Sentence
Finding elevated WBC ICD-10 on your report (usually D72.829) is concerning, but it’s almost always a sign your body is responding to something—often treatable. From common infections to stress or inflammation, most causes resolve with appropriate care. Serious conditions like leukemia are rarer but detectable with prompt evaluation.
At Prime Hospital Panipat, our hematology specialists offer thorough workups, accurate interpretation of elevated WBC ICD-10 results, and personalized plans. If your CBC shows high white cells or you’re feeling off, reach out—we’re here to help clarify, calm worries, and guide you toward better health.
Don’t wait if something feels wrong. Early attention makes all the difference.
